
With advancements in technology and a deeper understanding of type 2 diabetes (T2D), therapeutics, such as GLP-1 agonists and continuous glucose monitors (CGM), have significantly improved care options for patients with T2D. Despite these advancements, challenges for widespread effective care remain due to the heterogeneous patient population, opening the door for further development of treatments for T2D.
T2D & Obesity: Treatment Considerations
Acknowledging the T2D population as heterogeneous is essential for therapeutic progress since the origins vary widely. Obesity is a major factor in the prevalence of T2D, and it is vital to develop T2D treatments with this in mind. Evolving sentiments recognize obesity as a medical condition and lifestyle choice as well as a chronic disease with genetic, psychological, cultural, and environmental causes (Figure 1). Obesity-related conditions, including T2D, require a multifaceted treatment approach.
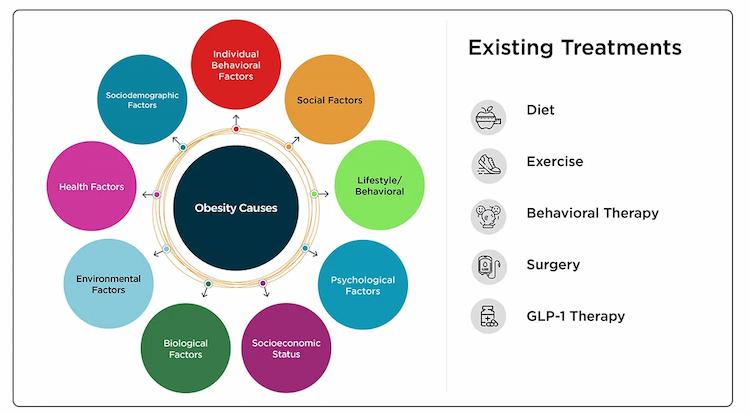
Figure 1: Obesity factors and current treatments.
A recent American Heart Association scientific statement highlighted a substantial gap between scientific evidence and clinical practice for effective obesity management, and this gap underscores the need for improved patient care models. Addressing obesity in the context of T2D requires a concerted effort from multiple stakeholders to dispel myths around personal responsibility for body weight, foster empathy for people living with obesity, and address underlying medical and environmental factors contributing to weight gain. Clinical development programs must acknowledge the complexity and variability of obesity as a condition. They should include a comprehensive set of outcomes and endpoints to capture multiple areas of potential improvement within obesity as a disease. Partnering with a CRO that emphasizes the complexity of the patient’s voice and harnesses the nuances of clinical trial design is crucial for executing successful clinical research.
The Role of Body Composition & Sarcopenia in T2D Treatment Development
T2D patient heterogeneity extends beyond etiology; body composition varies significantly between patients, independent of single metrics, such as BMI alone. Body composition metrics, therefore, require a comprehensive approach to measurement. For example, a retrospective chart review of T2D patients found that 28% of patients exhibited sarcopenia (loss of muscle mass), and 19% qualified as having sarcopenic obesity. Prevalence was more strongly correlated with body fat percentage than BMI, highlighting an essential difference in our understanding. In contrast, 55% of patients with “normal” BMI exhibited low muscle mass, and 34% of these patients with normal BMI also exhibited sarcopenic obesity, further diminishing BMI as a standalone and accurate readout for body composition and muscle mass. These data emphasize the need for precise and meaningful body composition endpoints in T2D and obesity clinical trials.
DEXA (Dual-Energy X-ray Absorptiometry) is the optimal method for accurately measuring body composition in clinical research. However, studies can use multiple methods to rigorously assess lean body mass, such as computed tomography (CT) scan analysis, musculoskeletal ultrasound, and bioelectrical impedance. DEXA is optimal for clinical research due to its standardization of procedures and comparability of results across studies (Table 1). CT scans and bioelectrical impedance may be preferable for screening, while ultrasound and bioelectrical impedance may be better suited for longitudinal clinical care.
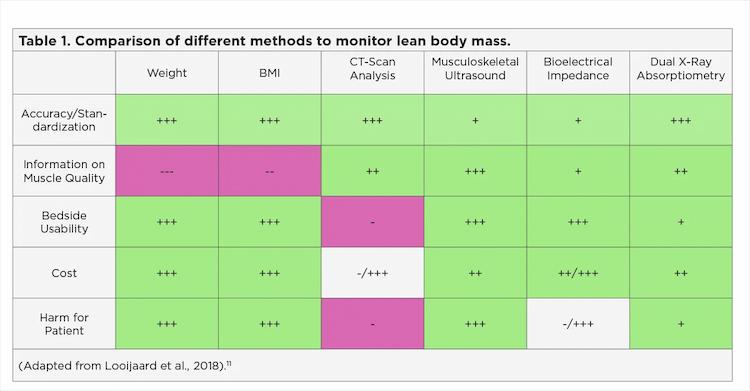
Table 1: Comparison of various methods to assess lean body mass.
GLP-1 Agonists & Emerging Technology
Regarding emerging treatments, regulatory bodies increasingly support GLP-1 agonists, which have shown preliminary efficacy for T2D and obesity management. These treatments offer cardiometabolic benefits and potential promise in mental health. However, the complex nature of T2D requires a multidimensional treatment approach that extends beyond drug therapy. Gene therapy, immunology, and CGM innovations provide new treatment possibilities. Research suggests that a combination of drugs and devices is most effective for managing T2D.
The Future of T2D Management
Effective T2D and obesity management requires innovative therapies, comprehensive patient care, and interdisciplinary clinical research. Emerging technologies and novel treatments promise improved patient outcomes but require careful consideration unique to relevant subpopulations. A patient-centric approach that emphasizes empathy, precision, and innovation is essential to advance the standard of care and encourage patients to follow intervention treatments more successfully. Interdisciplinary expertise, particularly in neuroscience, cardiovascular, and metabolic areas, is crucial for capturing the full potential of new therapies.
In our white paper, Advancing Type 2 Diabetes Management: The Importance of Interdisciplinary Expertise in Clinical Research, we provide an in-depth discussion about:
- Multifaceted interventions and employing a combination of current T2D therapeutics and technologies for optimal outcomes
- The role of varying body composition and impacts on T2D trial design and data interpretation
- Methods, tools, and trial-specific considerations for T2D research
- Neuroscience behind GLP-1 therapy and its potential as a holistic treatment approach beyond T2D and obesity
Contact us today to discuss your upcoming T2D or obesity trials with our experts!