
Next week, the Worldwide Evidence™ team will join colleagues and friends in Baltimore, MD, for the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) annual meeting. As a prelude to the conference, this blog covers several design best practices for building health economic models.

What is a Health Economic Model?
A health economic model is a mathematical framework designed to estimate the effects of a clinical treatment or intervention on valued health outcomes and costs. For example, a model of long-acting opioids for treatment of chronic non-cancer pain1 might extrapolate from available evidence (clinical trials, observational studies) to estimate the impacts of treatment on outcomes of interest to patients (quality of life, morbidity); employers (workplace productivity); healthcare systems (drug costs, adverse event costs); and/or societies (misuse, abuse).
To be useful, decision makers must have trust and confidence in a health economic model’s results. Health economic models impart confidence and enhance credibility in two main ways: (1) transparency, with clear descriptions of the model’s structure, equations, parameter values, and assumptions, and (2) validation, which compares the model’s results with events observed in reality.2
Sometimes the Bottom Line Doesn’t Matter
Health economic models provide decision makers with qualitative and quantitative information about decision problems. Certainly, models for understanding health care decision problems should reflect our best science, and a user’s ability to have confidence in a model’s quantitative results is paramount when prediction is the point of the exercise.
In some circumstances, though, users look to health economic models for other reasons – to make the relationships in a system explicit, to simplify complexity in order to allow deeper understanding, or to facilitate thinking that improves discussion. In these instances, there may be no right answer. There may be no bottom line, only possibilities and relative tradeoffs among alternatives. Many models exist simply to help decision makers identify these tradeoffs and to support intelligent discussion about possibilities. Ultimately, what matters for a health economic model is that it asks good questions and helps users explore good answers.
Good Modeling is Worth a Thousand Words
Transparency in health economic models is often difficult to achieve because we tend to approach modeling in the wrong way. It takes enormous craft, discipline, and experience to construct a health economic model, and modelers have developed meticulous, sophisticated methods to build them well. But modeling is not about methods. It’s about questions and answers. The methods are just the means.
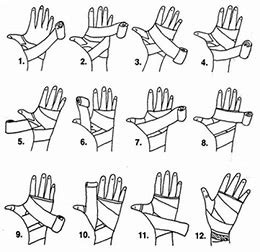
If a health economic model is intended to be evaluated, then it should be evaluable. If it is intended to be used, then it should be usable. Good design can facilitate this by enabling people to understand and process large amounts of information quickly, inviting them to think about substance without documentation standing in the way. Good design can communicate wordlessly, with clarity, precision, and efficiency. As a simple example, consider the wordlessness—and transparency—of Figure 1. Any written description of this diagram would, in all likelihood, be opaque to most readers.
Good architects—people who envision good buildings—know the difference between design and construction. Design explores different perspectives on the work: What will it do? Who is it for? In what context will it be used? How will we know if it’s successful? And then it integrates those perspectives into a plan. Construction is the act of building for reliability, integrity, and accuracy. Lacking design, even the most well-constructed health economic models can quickly become impenetrable academic exercises understood only by other modelers.
Social scientists have spent countless hours watching how people do things and studying how they think about what they do. Concepts from fields as diverse as cognitive psychology, learning theory, graphic design, visual analytics, and usability engineering have implications for enhancing the transparency of health economic models beyond the written word. For example:
- Conceptualize a health economic model to meet the need, not the other way around (marketing).
- Create a model with a logical flow the makes sense to the user (storytelling).
- Encourage new model users to persevere by helping them attain success from their initial actions (instant gratification and gamification).
- Allow users to proceed with an adequate, but perhaps not comprehensive, understanding of the model (satisficing).
- Make it easy to think through the component parts of the problem, rather than the whole problem at one time (incremental construction).
- Organize information according to users’ vocabularies and ways of categorizing concepts (spatial memory).
- Simplify tasks by splitting them into groups of operations, each of which can be addressed in a discrete mental space (chunking).
- Use visual cues to associate objects and ideas (grouping and alignment).
Let go of preconceived notions about how decision models are supposed to look. Form follows function! Any approach is acceptable if it solves the problem in an accurate, interesting way.
The challenge—and delight—is to realize the potential of these and other disciplines to transform a health economic model from a rarefied academic undertaking into a real-world tool. This transformation will come when there is a commitment by health economic modelers to work beyond the usual disciplines, embrace different approaches, and learn from the experiences of a variety of others.3
Health Economic Modeling and Real-World Evidence
If you would like to discuss this topic or other issues pertaining to real-world evidence, please contact the Worldwide Evidence™ team or stop by the Worldwide booth #238 at ISPOR 2018!
1 – Neil N, Merchant S, Provenzano D, et al. Clinical simulation model of long-acting opioids for treatment of chronic non-cancer pain in the United States. Journal of Medical Economics. 2012;16(2): 307-17.
2 – Eddy DM, Hollingworth W, Caro J, et al. Model transparency and validation: a report of the ISPOR-SMDM modeling good research practices task force—7. Value in Health. 2012;15:843-850.
3 – Neil N. Transparently, with validation. Medical Decision Making. Sept-Oct 2012:660-662


