In a major departure, the new Alzheimer’s disease (AD) research framework by the National Institutes on Aging and Alzheimer’s Association (NIA-AA) separates clinical symptoms from pathological state (1). This shift in thinking away from AD as a clinical-pathological construct and then as a clinical-biomarker construct (where biomarkers were used to support an AD diagnosis) represents the key feature to the updated research framework released in 2017 (2).
Talking Trials reviewed the updated research framework in a three-part blog series, featuring Natalia Drosopoulou, Ph.D., Worldwide’s Senior Director of Project Management in Neuroscience. The series concludes with this installment.
“How Updated Framework Impacts Alzheimer’s Disease Research – Part 1” covered the evolving definition of the disease and NIA-AA guidance on using biomarkers in research. Part 2 of “How Updated Framework Impacts Alzheimer’s Disease Research” discussed incorporating biomarkers that were excluded from the framework.
In the current research framework, AD is defined as a pathophysiologic construct that is uniquely and absolutely identified by biomarkers and that only biomarkers that are specific to AD proteinopathies (e.g., Aβ and pathologic tau) should be considered as potential biomarkers of AD. Therefore, AD can be viewed exactingly and exclusively as a proteinopathy.
As noted, several prominent biomarkers associated with proteinopathies, such as alpha-synuclein and TDP43, that play a crucial role in AD have been largely overlooked.
Beyond the biomarker issues noted earlier, are there other areas of concern in this updated framework for Alzheimer’s disease research?
Even if a manageable panel of a reasonable number of valid and reliable biomarkers for the AD continuum was widely recognized by the Alzheimer’s research community, it is important for AD drug developers to reconcile issues related to the cost and burden to both companies and to subjects (and their caregivers) with the apparent incremental increase in experimental control and internal validity that this framework might permit. Access to imaging and laboratory facilities varies greatly by geographic region, national health systems, and socioeconomic status. The authors of the framework recognize that it may not be feasible to obtain Alzheimer’s biomarkers in areas without access to the facilities or in populations less trusting of the health care system that are reluctant to participate in invasive clinical studies or even in low- and middle-income countries without adequate financial resources (1). This may be particularly problematic given the need to expand AD clinical trials into underrepresented populations and regions. This need is evidenced in a recent review we conducted of five global clinical trials in AD, which suggested that the vast majority of over 3,000 subjects were white and were randomized mostly from the North America and European regions.
Are there any other practical considerations for those engaged in Alzheimer’s disease research?
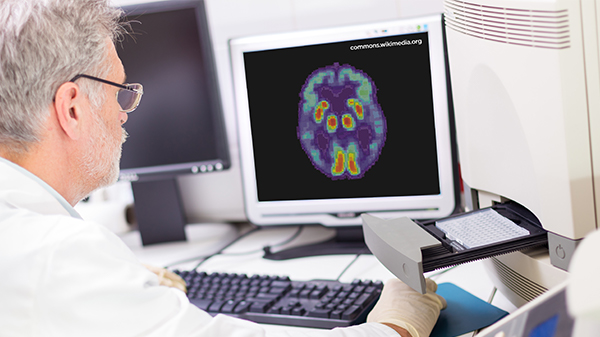
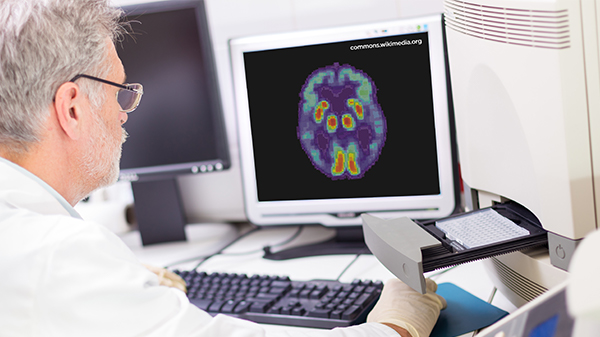
In terms of cost and burden, our experience suggests that most patients who participate in studies requiring PET imaging travel an average of 15-20 kilometers to reach an imaging center. When special PET ligands are required for imaging, the travel (and related costs) can be increased dramatically while the number of sites are diminished markedly because only clinical sites within the half-life of the tracer manufacturer can be utilized (typically sites within two hours’ drive time). In terms of costs, PET imaging considerably increases the total budget of the AD clinical trial and, depending upon the frequency of scans, can account for a large proportion of total Alzheimer’s clinical trial costs. The adoption of this proposed research framework will also undoubtedly increase the overall costs of AD trials due to increasing rates of screen failures owing to potential subjects not meeting biomarker criterion thresholds. It would not be unexpected to have screen failure rates as high as 75% in similar studies utilizing imaging and CSF biomarker criteria dependent upon specific inclusion criteria thresholds. It is possible to partially ameliorate such high screen fail rates using a hierarchic approach of a patient’s eligibility factors that takes into account all known and estimated screening variables. Following such a hierarchical procedure, our team has been able to reduce the screen failure rate in ongoing studies to well below the expected 75% rate to less than 50% (3).
Are there cases where this Alzheimer’s disease research framework would not be applicable?
Yes. That is possible, specifically in instances where biomarker data may not be essential for clinical investigation. The authors of the research framework concede that there may be Alzheimer’s research studies that do not require biomarker evidence of AD to achieve the specific goals of the research program, such as studies of cognitive decline or all cause cognitive dementia (1). Conversely, should regulatory agencies and/or ethics committees fully adopt this research framework, it may prove difficult for companies to maintain that biomarker evidence is not required for any and all registration efforts, and further, if biomarker data is required to define subjects for pivotal Alzheimer’s trials, it may also be reflected in eventual labeling, which affects the subsequent patient group eventually served.
Unfortunately, development programs that require biomarker validation of subjects (and conceivably these programs may be more likely to have novel mechanisms of action related to biomarker based drugs or devices) may end up only being available to large pharma who can afford these types of clinical studies, leaving non-biomarker-based programs to smaller companies. Access to and cost associated with biomarker acquisitions and analyses may actually serve as a disincentive to small companies seeking to develop novel drugs for the AD continuum. In summary, there may be numerous unforeseen practical consequences as well as far-reaching implications of a rapid and widespread adoption of this research framework that will require both careful consideration before and ongoing vigilance after implementation.
For more about the implications of the 2017 NIA-AA’s common research framework, read “Updated Research Criteria for Clinical Trials Across the Alzheimer’s Disease Continuum”.
References
- Jack CR Jr., Bennett DA, Blennow K, Carillo M, Dunn B, Elliott C, Haeberlein S, Holtzan D, Jagust W, Jessen F, Karlwash J, Liu E, Masliah E, Molineuvo JL, Montine T, Phelps C, Rankin K, Rowe C, Ryan L, Scheltens P, Siemers E, Siverberg N, Snyder H, Sperling R. 2018 NIA-AA research framework to investigate the Alzheimer’s disease continuum. Draft 7-18-17. http://alz.org/aaic/_downloads/draft-nia-aa-7-18-17.pdf.
- Riordan HJ, Drosopoulou NE. Updated research criteria for clinical trials across the Alzheimer’s disease continuum. Journal for Clinical Studies 9:5. 2017 November.
- Babic, T. and Riordan, H. Improving screen failure and recruitment rates in Alzheimer’s disease clinical trials. Journal for Clinical Studies 2016 Vol 8 (5):38-40.



