
Cardiovascular disease (CVD) has been the leading cause of death in the United States since the 1920s. Back in 2011, the American Heart Association (AHA) commissioned a report that showed that by 2035, upwards of 40% of the U.S. population would suffer from CVD. Sadly, we hit that mark 20 years early. The AHA recalculated the projected prevalence and economic burden of CVD out to 2035 in a study conducted by RTI International; the results are a haunting reminder that we still have work to do*. The number of Americans projected to have CVD by 2035 will have increased to nearly HALF (45.2%) of the U.S. population at 131.2 million. This means an additional 2 million cases of atrial fibrillation, 3 million cases of heart failure, 3.7 million cases of stroke, 4.2 million cases of coronary heart disease, and 27.1 million cases of hypertension.

Cardiovascular Disease Research Advances Offer Promise, Yet Progress Has Stalled
While CVD has been the leading killer of Americans for decades, advances in biomedical research, improved emergency response systems and treatment and prevention efforts helped improve morbidity and mortality in recent years, although without eradicating the disease or the downstream morbidity and mortality. Between 2000 and 2011, the national heart-related mortality rate declined at an average of 3.7 percent per year, while stroke mortality declined at 4.5 percent per year. The bad news is that since then, further progress has stalled. The burden of CVD is now on the increase due to multiple factors such as the dramatic rise in obesity and epidemic surge in Type 2 diabetes. In a reversal of fortune, the overall decline in CVD mortality rates has now flattened to less than 1 percent per year since 2011. In 2015, the death rate from heart disease actually increased by 1 percent for the first time since 1969, according to the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics.
CVD: America’s Costliest Disease
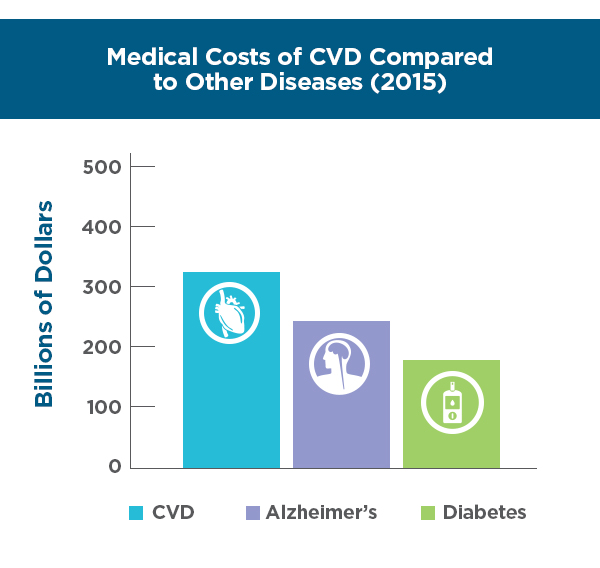
Further raising alarm, CVD is also now the costliest chronic medical disease in the U.S., with heart failure and stroke the most expensive chronic conditions in the Medicare fee-for-service program as of 2014. In 2016, costs related to CVD were $555 billion, and by 2035, costs are expected to exceed $1.1 trillion dollars – far surpassing medical cost estimates for other chronic diseases, such as diabetes and Alzheimer’s disease. Medical costs, in the form of hospitalizations, are expected to increase 135% to $749 billion, while indirect costs, such as in lost productivity, are projected to increase 55% to $368 billion. The biggest cost driver is the aging population, as CVD costs shift with the aging of the baby boomers. By 2035, CVD costs will more than triple in the 80 and older age group and more than double in the 65 to 79 year segment. CVD will maintain its place as America’s costliest disease. In fact, based on prevalence, death rates, disability and costs, CVD will continue to be the most burdensome disease Americans face today and in the future.
No Silver Bullet for CVD: Both Prevention & Treatment Are Key
So what is the solution? There is no one “silver bullet” solution for eradicating CVD. Investing in prevention through public health and wellness programs, while also driving access to new and improved treatments for CVD, will be essential to reducing the impact of this disease. This means ongoing investment in research and development related to CVD; however, to date, the National Institutes of Health invests a mere 4% of its budget on heart disease research, 1% on stroke research, and 2% on other types of CVD research. This is while heart disease and stroke account for 23% and 4% of all deaths, respectively.
Achieving a decline in CVD mortality and morbidity through prevention and new treatments will not only lengthen and improve the lives of many around the world, but declines will also trickle-down and have a beneficial effect on the global economic burden, by reducing the major drivers of direct and indirect costs due to CVD. Pharmaceutical and biotechnology companies, along with contract research organizations, are working collaboratively with regulatory entities around the world to find ways to bring new treatments to market more quickly, and cost effectively (read more in my Part 1 and Part 2 of my earlier blogs on innovative trial design).
While there is no “silver bullet” to progress in CVD, as a cardiologist and a clinical researcher, I am proud to be a part of this industry and working collaboratively with our customers who are uncovering innovative approaches to cardiovascular disease research, and I am confident that one day soon we can once again achieve CVD mortality and morbidity declines in the U.S. and around the world.
*RTI International (commissioned by the American Heart Association). Projections of Cardiovascular Disease Prevalence and Costs: 2015–2035. November 2016.


